Mycosis fungoides can progress slowly through several stages. In the early stage, you develop flat, scaly patches of skin that may be itchy. These patches may disappear and reappear, or stay the same size for years.
The PDQ cancer information summary for mycosis fungoides (including Sezary syndrome) provides comprehensive, up-to-date information about the disease. It was reviewed and updated by health care professionals.
Patches
A scaly skin rash that is usually itchy may develop on parts of the body protected from sun exposure, such as your lower belly, thighs and butt, armpits and groin. It can also appear on other areas of the body, including your face. The rash can grow, become thick and form patches or plaques. The rash often develops sores that may heal or ulcerate.
The rash may be different colors, ranging from tan to red and brown. The rash is usually dry and itchy, and it often gets worse when you scratch it. Itching is a key sign of mycosis fungoides, but it’s not the same for everyone. Some people with mycosis fungoides have little or no itching at all.
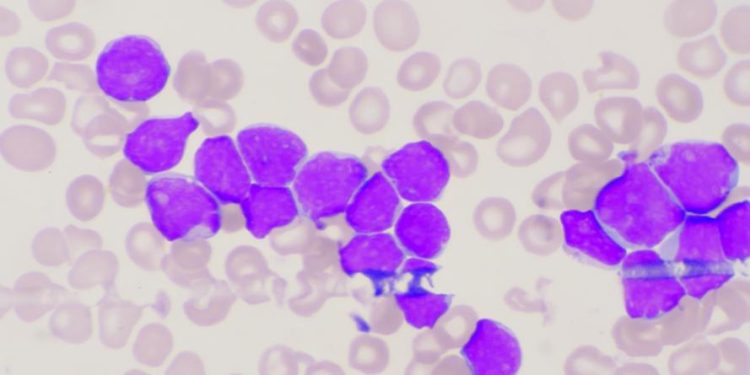
Classic mycosis fungoides (MF) progresses slowly over years from patches to plaques and eventually to tumors. It is the most common form of cutaneous T cell lymphoma, accounting for about 50 % of all primary cutaneous T-cell lymphomas. MF is characterized by infiltrates of malignant T lymphocytes, with a tendency to clonal expansion and irregular cerebriform nuclei.
During the patch phase, there is a superficial lichenoid infiltrate containing mostly lymphocytes and histiocytes, with occasional atypical cells. This is similar to other lichenoid dermatoses and can be difficult to distinguish from eczema or other inflammatory skin diseases. MF in the patch phase is rarely spread to other organs.
When mycosis fungoides moves to the plaque stage, there is a dense dermal infiltrate containing many small to medium sized malignant T lymphocytes with irregular cerebriform nuclei and a tendency for expansion. Some lesions contain sores, but most do not. MF in the plaque stage is sometimes spread to other organs, including the lymph nodes and liver.
The disease is hard to cure, but treatment can ease symptoms and improve your quality of life. Treatment is based on the stage of the disease, the type of skin lesions and whether any tumors are present. Blood tests can help assess your overall health and check for other cancers or blood conditions that can affect your treatment. A test to look for changes in the genes that make the T cell receptors can help identify the type of MF you have and what treatment you might need.
Plaques
Most people with mycosis fungoides go through a stage of patches and plaques before the disease gets worse. A small proportion of people get raised lumps called tumors, which may ulcerate or weep. These are the most serious signs of mycosis fungoides, and are the reason why it is important to see your doctor if you have them. They are also a sign that the lymphoma may be spreading to other parts of your body.
The classic mycosis fungoides, which usually occurs in middle age or older, starts as flat, scaly patches of skin that look like a sunburn. It often occurs in areas of the body that don’t get much sun, such as the back, stomach, chest and buttocks. These patches and the surrounding skin can itch. Sometimes the skin becomes thicker, redder and more painful. It is then known as Sezary syndrome. It is very rare for mycosis fungoides to spread beyond the skin to other organs.
Other forms of mycosis fungoides occur in younger adults, and are less serious than the classic form. Folliculotropic mycosis fungoides (MF) may cause itchy, follicular papules that are shaped like hair follicles, and they tend to affect the scalp and neck. The rash is usually more widespread, and the lymph nodes in the neck can become inflamed, enlarged and painful (lymphadenopathy). The plaques may also appear in other places on the body.
Another rare form of mycosis fungoides is poikilodermic mycosis fungoides, which develops in people with darker skin tones. It is characterized by a combination of scaly patches, itching and telangiectasia. It is not known why this subtype of mycosis fungoides develops more commonly in people with dark skin.
Hypopigmented mycosis fungoides may also occur, and can look like a very light psoriasis or vitiligo. This type of MF is less common, and it may be harder to diagnose than the more common types of mycosis fungoides.
Mycosis fungoides can be treated with psoralen plus ultraviolet A, an immunosuppressive drug that suppresses your immune system. Other drugs that can be used to treat mycosis fungoides include doxorubicin, cyclophosphamide and methotrexate. There are a number of treatment clinical trials being carried out to test newer treatments for mycosis fungoides and Sezary syndrome. You can talk to your doctor about whether taking part in a trial could benefit you.
Tumors
If mycosis fungoides gets worse, it may affect your internal organs, such as the lymph nodes and liver. This is a serious stage of the disease and may cause symptoms such as itching, fever, weight loss and weakness. The cancer can also spread to other parts of the body, such as the brain.
During mycosis fungoides, the cancer cells grow and develop tumors. These are often large and itchy, and they may be covered with thicker skin. Tumors can form on the skin or in the lymph nodes, and they may be found all over your body. In some cases, tumors can affect the heart, kidneys and lungs.
Your doctor will diagnose mycosis fungoides with a physical exam, a blood test and other tests. These include a CT scan and blood tests that look at your immune system and the number of cancer cells in your body.
Doctors haven’t identified a single cause for mycosis fungoides, but they believe the disease is caused by changes in certain genes. These changes may happen quickly (acquired) or over time (chronic).
If you have mycosis fungoides, your doctor will probably recommend treatment based on the stage of your disease. The first stage is called stage 1A and is when the rash has patches or plaques, but the cancer hasn’t spread to the blood or lymph nodes. The first stage usually improves with treatment.
The second stage is called stage 2 and happens when the patches or plaques have grown bigger or cover more than 10 percent of your body. You might also have enlarged lymph nodes in your neck or armpits. The most common treatments are methotrexate, doxorubicin and radiation therapy.
Radiotherapy uses high-energy X-rays to destroy cancer cells in the affected area. It can be used to treat specific areas of the skin, or it can be given to your entire body surface. You may be prescribed drugs to control the cancer, such as bexarotene tablets, which belong to a group of medicines known as retinoids. You can find more information on these in the British Association of Dermatologists patient information leaflet on bexarotene. You may be given chemotherapy to kill the cancer cells in your blood, such as cisplatin and fludarabine. You might receive immunotherapy, which involves boosting your immune system to attack the cancer cells. This is a newer treatment that’s still being researched.
Treatment
Mycosis fungoides can be difficult to diagnose. It usually starts as scaly, itchy patches that can be flat or slightly raised and are often mistaken for common skin conditions like psoriasis or eczema. The patches can disappear, stay the same size or enlarge over time. Occasionally, the patches can develop sores that break open and bleed. The condition can also be very itchy and some people have long-term, generalized itching (pruritus). In very rare cases, mycosis fungoides can spread to other parts of the body and may cause symptoms in other organs.
Most cases of mycosis fungoides are stage I, meaning the lymphoma affects only the skin and has not spread to other parts of the body. However, mycosis fungoides and Sezary syndrome can recur (come back) in the skin or in other organs like the liver and spleen after treatment.
Some treatments can help prevent mycosis fungoides from coming back or spreading. These include medication and radiation. Your doctor may recommend a combination of these treatments or clinical trials that are testing new ways to treat mycosis fungoides.
There is no cure for mycosis fungoides once it has spread to other parts of the body, but treatments can control the condition and help you feel better. It is important to get diagnosed and treated early. In a 2022 research study, people who were diagnosed in the earliest stages of mycosis fungoides had a 95% chance of survival over 10 years.
The following treatments can be used for mycosis fungoides:
The most common treatment is a course of chemotherapy. This involves taking several anticancer drugs that destroy cancer cells in your body. There are many different types of chemotherapy drugs and they work differently in different people. You might also receive other therapies such as photopheresis, allogeneic stem cell transplant or radiation. You can find more information about these treatments and other options in this PDQ cancer information summary.